

International Journal of Physiotherapy Research and Clinical Practice
DOI: 10.54839/ijprcp.v4i2.25.23
Year: 2025, Volume: 4, Issue: 2, Pages: 1-7
Original Article
Routhu Hari Guruvulu1,∗, Suman Kumar Tadagonda2, Naresh Kumar Pagidimarry3, Tejaswini Damerla4, Vamshi Krishna Pasupuleti1, Nikhitha Samala4, Mahesh Babu Bellam4, C H Kavya4, Vishnu Vardhan Rao4, Krupa Rao Palle4, Mayuri Chandra Basude4, Abhishek Vadlakonda5, Sukumar Sura6
1Spine physiotherapist, Centre for Spine and Sports Health (CSSH), Gachibowli, Hyderabad, Telangana, India
2Sports medicine physician, Centre for Spine and Sports Health (CSSH), Gachibowli, Hyderabad, Telangana, India
3Managing Director and CEO, Centre for Spine and Sports Health (CSSH), Gachibowli, Hyderabad, Telangana, India
4Spine physiotherapist, Nsure healthy spine, jubilee hills, Hyderabad, Telangana, India
5Operations Manager, Centre for Spine and Sports Health (CSSH), Gachibowli, Hyderabad, Telangana, India
6Chief of Neurosurgery, Asian Spine Hospital, Jubliee Hills, Hyderabad, Telangana, India
*Corresponding Author
email: [email protected]
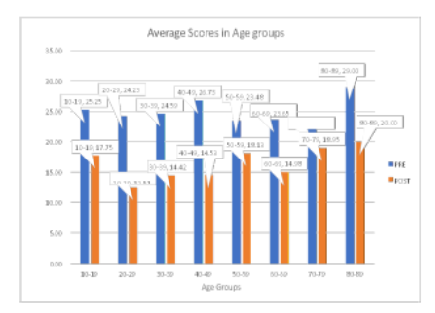
Spine-related disorders are among the leading global causes of disability, with increasing prevalence across all age groups due to sedentary lifestyles, poor posture, and age-related degeneration. There is a growing need for targeted interventions that address functional limitations through individualized care. This study evaluates the effectiveness of age-specific, personalized spinal interventions in a cohort of 3,000 patients treated at a dedicated spine health center. Functional outcomes were assessed using the Oswestry Disability Index (ODI), a validated tool for measuring spine-related disability. A total of 3,000 patients underwent comprehensive assessment and individualized treatment based on age, functional impairment, postural anomalies, and diagnostic imaging. Pre- and post-treatment ODI scores were compared across age groups (10–89 years). Data were analyzed for trends in baseline disability and improvement rates. The overall mean ODI score decreased from 24.53 to 15.35, representing a 37.4% improvement in functional status. The most notable improvement was seen in the 20–29 age group (48.4%), while the 80–89 group also exhibited a meaningful 31.0% improvement despite high baseline disability. A U-shaped pattern in baseline scores was observed, with higher disability in both younger (10–19) and older (80–89) cohorts. Age-stratified analysis revealed that tailored interventions yield substantial functional improvements across the lifespan. Younger patients respond more robustly, yet older adults also benefit significantly from structured rehabilitation. These findings advocate for individualized, age-sensitive treatment models and emphasize early intervention and functional goal alignment for improved outcomes in spinal health
Keywords: Spine health screening, Oswestry disability index ODI, Age specific rehabilitation, Personalized spine care, Functional outcomes, Postural and radiological assessment
© 2025 Published by Krupanidhi College of Physiotherapy. This is an open-access article under the CC BY license (https://creativecommons.org/licenses/by/4.0/)
Subscribe now for latest articles and news.